Some Wondrous Discoveries to Come
A new future for medicine with stem cells
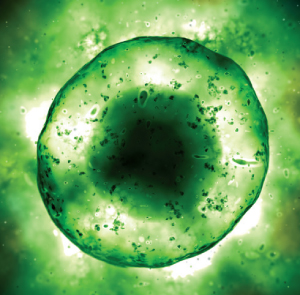
In the earliest days of our existence, each of us is not much more than a microscopic cluster of identical cells rapidly reproducing inside a thin membrane, each cell containing the full potential for what we will become.
Then they “differentiate.” Like freshfaced high school graduates, these cells, called pluripotent stem cells, choose their divergent paths in life. Genetic cues kick in, and some cells give rise to brain and nerve tissue; others, to muscle, bone, blood, vital organs and skin.
One of the greatest quests of contemporary science is unraveling the mystery of how these early cells make those leaps. Harnessing that power, scientists say, offers a new future for medicine, with new hope for people who suffer devastating spinal cord injuries, deadly organ failures or heartbreaking brain conditions like Parkinson’s and Alzheimer’s diseases. The day may come when medicine can nurture these stem cells into growing replacements for diseased tissues.
the potential for turning UTSA and San Antonio into a global hub for research and development of cutting-edge therapies for a multitude of diseases. That is the vision of UTSA stem cell biologists John McCarrey, Ph.D., and Chris Navara, Ph.D. They are working with San Antonio’s Texas Biomedical Research Institute and Harvard University to develop an animal model that can be used to probe the workings of pluripotent stem cells and test the safety and effectiveness of new therapies that will emerge. Stem cells can become any tissue in the body. As adults, humans produce some stem cells that can repair some tissues in the body. But the most powerful cells are the undifferentiated stem cells produced in the embryo a few days after conception.
Inducing Pluripotent Cells
Japanese scientists in 2006 discovered how to induce ordinary mouse cells into turning back the clock and becoming pluripotent again. The following year, independent Harvard and Japanese teams showed they could get human cells to do the same thing.
This was a major scientific breakthrough. It gave scientists a way to avoid the ethical controversy of experimenting with human embryonic stem cells—experiments that destroy the embryo in the process. It also showed the potential for so-called regenerative medicine, in which a patient’s own cells may someday be coaxed into growing the specific body tissue that he or she needs to repair a damaged heart, brain, liver or other organ. The body’s immune system should recognize the implanted tissue as its own, avoiding the common and dangerous problem of rejection that now comes with transplant surgery.
But the discovery of induced pluripotent cells is just the tiniest crack of light coming through the doorway. Scientists still have much to learn about how these cells work and how to turn them into safe and effective medical treatments.
“We believe there needs to be a good preclinical animal research model system for the study of stem cells,” McCarrey says. “For all their promise, there still are a lot of questions to be addressed before we start putting them into people.”
Texas Biomed, until recently known as Southwest Foundation for Biomedical Research, is home to the federally supported Southwest National Primate Research Center. Since the 1950s, scientists there have studied baboons as a model for chronic human diseases like diabetes, atherosclerosis, obesity and arthritis. The institution has a pedigreed colony of about 1,500 baboons for which there are complete family and medical histories as well as a genetic linkage map. That makes the animal a powerful model for studying both basic science and clinical applications of stem cells, the scientists say.
“For example, how do we get stem cells to the right place?” McCarrey says. “How do we get them to express the correct genes? Do they fix the problem? Can they cause cancer? There are similarities between stem cells and cancer cells. We need to study this in an animal model.”
Mice, the standard laboratory animals for early phase studies, are just too different from humans to be used for all preclinical studies. Baboon immune systems more closely resemble those of humans, and the animals live many years longer than the typical laboratory mouse and can help researchers understand the long-term implications of these treatments. “We need a long-lived model that we can do long-term follow-up on,” Navara says. “That is definitely not a mouse.”
Navara, a cell biologist who joined the UTSA faculty in 2008, is most interested in developing mesenchymal stem cells from pluripotent stem cells. These cells will go on to form bone, cartilage and fat.
He also is studying two key proteins, Aurora B and Survivin, which are particularly abundant in both stem cells and numerous types of cancer cells. This is one of a number of worrisome similarities between stem cells and cancer cells. “All of them must be understood before stem cell therapies can be safely used in human therapies.”
“We need to understand, what is the function of these proteins? Why do the stem cells make so much?” Navara says. “We are studying how these cells divide. One of the things that cancer cells do is lose or gain chromosomes, and embryonic stem cells do the same thing.”
Animal Studies to Help with Stem Cell Therapies
UTSA, Texas Biomed and Harvard have formed a partnership called PriStem, which is seeking a federal grant to support their plans to use the baboon as a research model for stem cell therapies. They envision a national resource that would be available to scientists everywhere. This would allow clinical experts in diseases like diabetes or in brain trauma to collaborate with San Antonio investigators on animal studies to help them develop and evaluate the safety of stem cell treatments for any number of conditions.
“This would be huge for San Antonio,” McCarrey says. “This would draw new private investment, new federal grants, new companies. And health care already is a large part of the regional economy.”
McCarrey heads a new Institute for Molecular and Cellular Primatology, a collaboration between UTSA and the University of Texas Health Science Center, through which clinical experts, basic science researchers and biomedical engineers are already working together on a number of early-stage projects.
UTSA is building faculty expertise and expanding student programs in this cutting-edge field as well. It has recruited two new scientists—Brian Hermann, Ph.D., who has expertise in reproductive biology, and Annie Lin, Ph.D., who is interested in the potential applications of the neural stem cells that build brain tissue.
Student opportunities are expanding as well, as researchers add master’s and doctoral level positions in their laboratories. “This is an area that students are finding attractive,” McCarrey says.
“We are going to have some amazing opportunities here. Some amazing discoveries, too.”
Error processing SSI file