The battle to reduce the deaths caused by nosocomial, hospital-acquired, infections has reached San Antonio. And the new battle lines are being drawn right here at the UTSA College of Engineering. Under the guidance of biomedical engineering professor Anand Ramasubramanian and biology professor Jose Lopez-Ribot, Ph.D. student Anand Srinivasan is creating a faster, more cost-effective way to test drugs on fungal biofilms. His work could allow doctors to test thousands of drugs within hours rather than days, saving both money and lives in the process.
People expect hospitals to be clean, safe and a place to heal. But what if the hospital isn’t clean? What if it isn’t safe? What if, instead of healing, a patient dies? That’s the nightmare scenario UTSA’s Anand Ramasubramanian, Jose Lopez-Ribot and Anand Srinivasan are working to end.
According to the Centers for Disease Control, approximately 1.7 million nosocomial, or hospital-acquired infections (HAIs), from all types of microorganisms, including fungus, cause or contribute to 99,000 deaths every year in the United States. The development of such infections is actually facilitated by a hospital environment and can be transmitted to patients whose resistance is compromised.
While the medical community is fighting back, testing thousands of fungal biofilm samples gathered from hospital surfaces throughout the world is time-consuming and costly.
When Ramasubramanian, a biomedical professor and expert on high-throughput medical sample analysis, and Lopez-Ribot, a biology professor and pioneer in the field of fungal biofilms, met an idea was born. What if they could combine their research to develop a way of processing thousands of fungal biofilm samples at a time? It could be a game changer.
"It was clear we needed better drugs to treat the infections caused by fungi," explains Lopez-Ribot. "Fungal biofilms is a field I’ve been working in for a long time and the one thing that has been stopping me from working faster is technology. The expertise Dr. Ramasubramanian provided with his cellular chips was the perfect scenario to combine with my expertise."
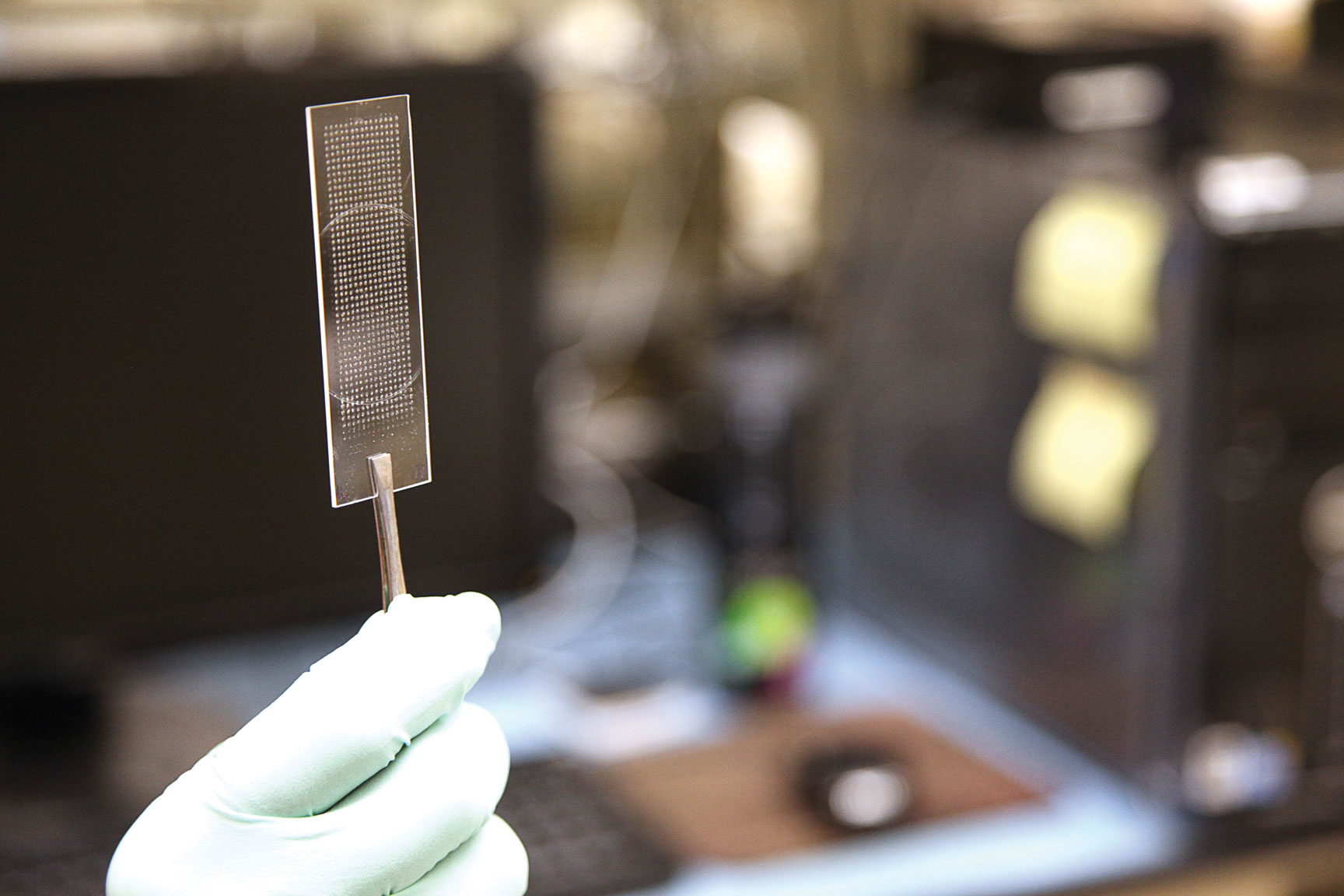
Srinivasan, a biomedical engineering doctoral candidate who came to UTSA from India for the opportunity to work directly with the university’s professors on healthcare-related research, was enlisted based on his work on a chip capable of holding thousands of fungal biofilm nanocells which could then be tested against various drugs.
The previous process required technicians to use pipets to place sizeable samples into a 96-well tray which was then tested by hand. The backlog created by the enormous volume of samples to be handled could delay test results by up to a year.
"A high-throughput technology offers a robust platform for rapid, cost-effective, easy handling and automated analysis," says Srinivasan. "Compared to the current technology, our chip technology is controlled by a robotic printer that prints cells, drugs and uses 2,000 times fewer reagents while still providing reliable results. One such chip is equivalent to a dozen 96-well plates, so imagine the number of experiments that could be done using one chip."
While their current project focuses on fungal biofilms, there is nothing stopping the threesome from expanding into other areas of microbial research. The multidisciplinary project can be applied to the process of drug discovery for any pathogen or mammalian cell model. For Srinivasan, who developed the process and is amazed by its potential, the work is a bit more personal.
"I call it ‘the next generation’ of in vitro assay platform for drug discovery," Srinivasan explains. "The CaBChip is a powerful and revolutionary model in identifying novel drugs from large drug libraries, with a potential of changing the phase of conventional high-throughput screen strategies. This model can be extended to high-throughput assays, enzyme inhibition and cytotoxic assays of all microbial flora of fungi and bacteria."
Based on preliminary estimates, the cost of drug testing will be a tenth of what it is right now, and increasing the speed of drug tests means patients can receive medical care faster than ever before.
The work done by this UTSA team is, indeed, a game changer.